Receiving a cancer diagnosis can feel as if you are stepping into the unknown. We often receive questions about how to prepare for different types of cancer treatment – and chemotherapy is usually top of the list. We turned to our Shine Cancer Support community members and asked them to share their tips on making it through chemo and we’ve compiled them below. Knowledge is power so read on for our top ten tips…!
1. Ask what to expect from your treatment

Ask what to expect – it may not be as bad as you were thinking!
Cancer isn’t one disease – and chemotherapy isn’t ‘one size fits all’ either. Before you start treatment, ask your doctor or nurse for specific details about the drugs that you’ll receive. Will you need to take tablets, or will your treatment will be given intravenously? If you need to go to hospital for treatment, how long can you expect to be there? Once you’ve had the treatment, what side effects can you expect? What should you do if you feel unwell? Will your treatment affect your fertility? It can be helpful to sit down with friends or family and brainstorm a list of questions that you would like to ask your medical team. It might sound like a cliché, but there really is no such thing as a bad question. There may well be things you’ve never heard of before (hello mucositis!) but forewarned is forearmed and it’s better to know what might happen so you can be prepared to manage it.
2. Plan your time on the ward
It can be daunting to walk into a treatment centre for the first time. Before your first treatment, you might find it helpful to know a bit more about the place where you will be treated. Does the ward have wifi, for example, or a TV? What is the visiting policy? Do you need to bring snacks or will food be provided? You can usually get answers to these questions from your specialist nurse, or by calling the ward secretary. If you have time, you could also pop your head around the door of the ward before your treatment and see what it’s like.

Waiting around can be BORING. Don’t just lie there – watch Netflix!
Shine member Neil advises looking at your data plan if your hospital doesn’t have good wifi – you might want to purchase extra in advance, or get a mobile wifi device. You don’t want to find yourself out of 4G halfway through your Netflix series!
3. Plan your journey (there and back!)
Running late can add even more stress to a situation that’s difficult enough! Take a moment to work out how to get to hospital for your treatment. Can someone drive you there, or will you need to take public transport? If you’re driving, do you need to pay for parking? Shine member Tracey recommends checking with your medical team: some hospitals offer free or discounted parking to patients who are in regular treatment. If you’re in London, consider if and when you’re going to take public transport to and from your appointments. Cancer on Board will send you a free badge to wear while TfL also provides free “Please offer me a seat” badges – don’t be embarrassed! You deserve a seat!

Tablet and phone recommended!
4. Treat it like a long-haul flight
When asked members of our Shine community what advice they would give to others who are about to start chemotherapy, this was the overwhelming consensus: pack a bag with all the things that you’d take on a long plane journey. Books, puzzle books, a laptop or tablet, fluffy socks, and a nice jumper or cardigan were all on our list! Shine member Christine highly recommends headphones: ‘even if you don’t want to listen to music/watch something on your tablet, you might need them if you get stuck next to an annoying person…!’
5. Track your side effects
Your medical team will want to know how you are doing between treatments. Keep a notebook with details of any side effects that you experience, so that you can give accurate information to your doctor. If notebooks aren’t really your thing, you could also use try note-taking apps. And don’t be shy about mentioning side effects – a lot of things can be managed with medication or the right support. Don’t suffer in silence!
6. Get some fresh air
Shine member Samantha found getting outside to be really helpful when she was having chemotherapy treatment: ‘even on the days when you are as weak as water, a toddle in the garden or wander up and down the street will give you fresh air, confidence in moving about and sense of accomplishment.’ Exercise has been shown to benefit people with living cancer (let’s face it – exercise benefits everyone!), but it can be difficult to know where to begin. If in doubt, ask your medical team for advice. If you exercised regularly before your cancer diagnosis, you might also want to look at cancerfit.me, a new community created by doctors and athletes with an interest in sport and fitness for cancer patients. And you can also read our blogs about how running, cycling and yoga have helped Shine members through treatment.
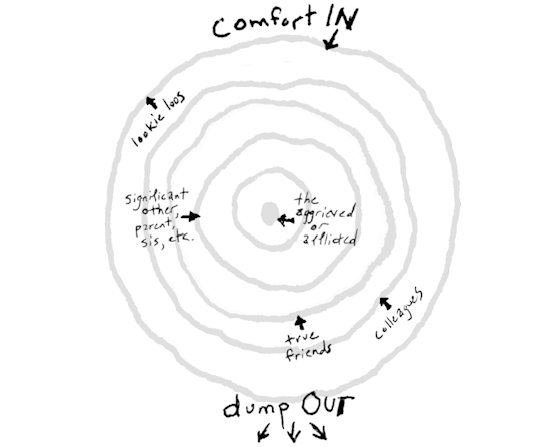
7. Get help!
It can be difficult to cope with a cancer diagnosis by yourself. Mobilise your team! You might find it helpful to ask a close friend or family member to co-ordinate those who come forward with offers of help. Specific offers of help are often easiest to take up, but many people struggle to know what to do when they hear that someone they love has been diagnosed with cancer. If you can, make a list of things that might be helpful and share this with a friend/friends. Do you need someone to make you meals, for example? Or someone to walk your dog? Would a visit from a friend make your week? Let them know! You can direct them to our blog about ways to help a friend with cancer – and you can direct them to our post on what to say to people with cancer while you’re at it!
8. Prepare yourself for bad days
Some people sail through cancer treatment with very few side effects, while others can find themselves cowering under a duvet for days after treatment. Shine member Stewart says: ‘plan for the side effects… BUT don’t get drowned in the gloom of EXPECTING them all. Everyone’s experience is different, so know about things like the possible options for creams, gloves, hair shaving, food to ease/slow bowels, support networks etc.’ Your doctor or nurse will be able to provide you with specific information about how to treat side effects from your drugs. And, as hard as it is, remember that they won’t last forever.
9. Don’t forget the good days
More wise words from Stewart! He recommends that you also ‘plan for the time in-between.’ You may have to manage expectations around what you can do, but that shouldn’t stop you from having fun! Shine member Caroline keeps a list of things that she’d like to do on good days: ‘I have a list of new cafes or restaurants that I’d like to try, and places that I’d like to visit on day trips. They’re all options, rather than firm plans, but on good days I love to scan the list and pick out something fun to do.’
10. Listen to your body
Receiving a cancer diagnosis can make you much more in tune with your own body. Are you suddenly noticing lots of niggling aches and pains that you swear weren’t there before? Join the club! If you have any concerns about your health, contact your medical team – that’s why they’re there! If you’re feeling tired, perhaps think twice about going on that big night out and invite a friend over to spend the evening with you instead. By the same token: if you wake up in the morning and feel well, embrace it! Life doesn’t have to stop when you have cancer.
Cancer can make you feel lonely. If you’d like to chat to other young people with cancer and share more tips and tricks about how to cope, join our private Facebook group Shine Young Adult Cancer Support (20s, 30s & 40s). You can find out more about all the support we offer via our website.
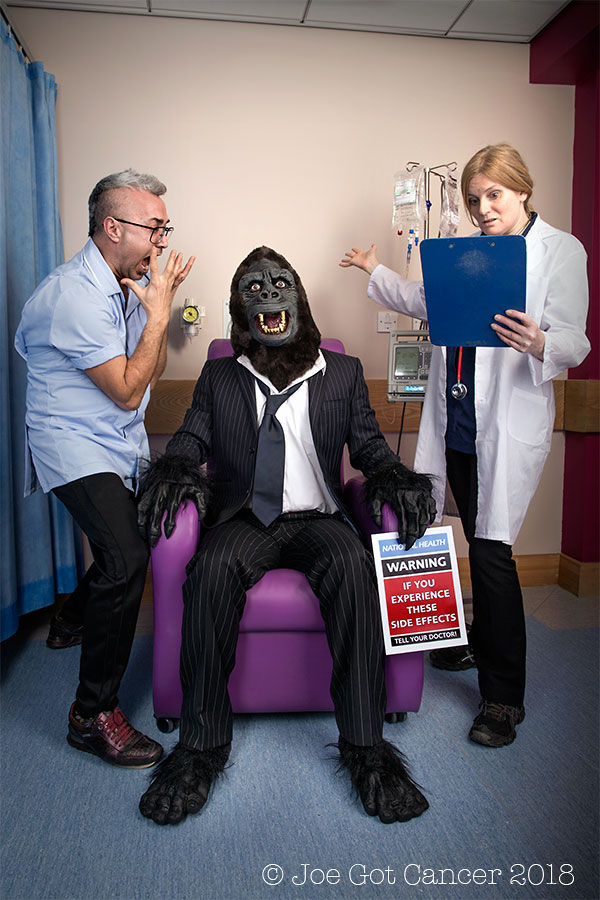
Special thanks to Joe Hague for letting us use his photo (above!). If you’d like to learn more about his photography, please check out his Facebook page or his Go Fund Me page.